Implicit bias refers to instances of stereotyping that occur unintentionally or unconsciously. This type of bias occurs during all forms of social interactions and has been a topic of inquiry for social and behavioral scientists for decades. The research generally discusses implicit bias as resulting from learned stereotypes that are often ingrained into our judgements of others in early life. Importantly, even when explicit beliefs about a group evolve over time, implicit bias persists.
For example, 2013 research from Chapman, Kaatz, and Carnes shows those who report egalitarian attitudes may still display implicit biases related to racial and gender minorities. While stereotypes may help people process information more quickly, they often also lead to misjudgment of individuals based on group-level perceptions. Because physicians are trained to understand health and medicine at the group level, they may easily rely on stereotypes for decision-making, bringing implicit bias into their medical practice.
Implicit Racial Bias in Pain Medicine
Hoffman and colleagues’ 2016 study may be the most well-known piece of research demonstrating implicit racial biases in clinical evaluations of pain. Through an experimental survey design manipulating the race of patients to be either white or Black, the authors reveal that medical students and residents who endorse false beliefs of biological difference between Black and white people also rate Black patients’ pain as less intense than white patients’ pain.
Other researchers have noted similar differences between other marginalized groups of patients and white patients. For example in a 1993 study, researchers Todd, Samaroo, and Hoffman found that Hispanic patients had higher odds of not receiving pain medication for long-bone fractures compared to non-Hispanic white patients in the UCLA Emergency Medical Center. Further, Anderson and colleague’s 2009 review on the racial and ethnic disparities in pain literature shows Asian patients received significantly lower opioid doses for their post-operative pain compared to white patients.
Gender Biases in Pain Assessment and Treatment
In a 2001 review of a separate line of literature on gender biases in pain assessment and treatment, Hoffman and Tarzian demonstrate a gender bias in how pain is assessed and treated during medical encounters. For example, compared to men, women are more likely to be given sedatives, rather than pain medication, for their pain.
This difference in medication distribution suggests that women’s pain is often assumed to result from psychological factors, rather than somatic conditions. Men and boys are also more likely to receive pain medication postoperatively, compared to women and girls. Additionally, one study reviewed by Hoffman and Tarzian demonstrates that women endure pain longer than men before being referred to specialty pain clinics.
Understanding implicit biases related to pain evaluations is important because such biases impact the diagnoses patients’ receive and therefore the treatment options available to them for managing their pain. The research I conducted on pelvic pain evaluations expands upon what social scientists have previously discovered by providing more context on implicit biases and the various ways they manifest during pain evaluations.
The Research
As a sociologist who has spent nearly a decade studying health inequality, I know that one of the major fundamental causes of health inequality is SES. As a gender and intersectionality scholar, I also know that gender and race have an undeniable impact on the our interactions with other humans, even in medical settings as the research on pain biases tells us. Therefore, I set out to understand not only more about gender and racial biases related to pain assessment but also biases related to SES and how all these biases intersect to impact patients differentially.
To do so, I designed a survey experiment using methodological techniques to allow for evaluating the causal impact of these biases on evaluations of patient pain. That means I could isolate factors like patient race, gender, or SES as the factor(s) impacting certain evaluations. Using statistical methods and software, I also evaluated how the combination of a patients’ gender, race, and SES impacted their evaluations. Doing so gave me the ability to answer questions like, do Black, high-SES, male patients receive more or less favorable evaluations of their pain compared to white, low-SES, female patients?
Those who responded to the online survey and thus provided the evaluations of patients were healthcare workers in the US, including a total of 453 providers, nurses, and other support staff working in healthcare settings. Participants were presented with three patient intake forms of fabricated patients and were tasked with answering seven questions about each patients’ pain including evaluating the level of the patient’s pain from 1-10, the seriousness of the patient’s pain, and the likelihood of referring the patient to a specialist. Participants were also asked a set of questions regarding their endorsement of false statements regarding race and health, and gender and pain.
Results on Implicit Bias
Gender Biases
A whole 73% of survey respondents working in healthcare settings falsely believe women, on average, can tolerator more pain than men. Roughly 53% of survey respondents also falsely believe that women are more susceptible to psychosomatic pain—or pain caused by psychological conditions like stress and anxiety—compared to men.
It may be unsurprising then that research shows female patients typically wait 5-10 years to receive a diagnosis for endometriosis, just one of a long list of conditions causing persistent pelvic pain. Relatedly, and perhaps unsurprisingly, the survey respondents rated female patients’ pelvic pain as significantly more typical, or normal, than male patients’ pelvic pain suggesting a normalization of women’s pelvic pain that often impedes their ability to receive adequate diagnoses and treatment.
Socioeconomic Status Biases
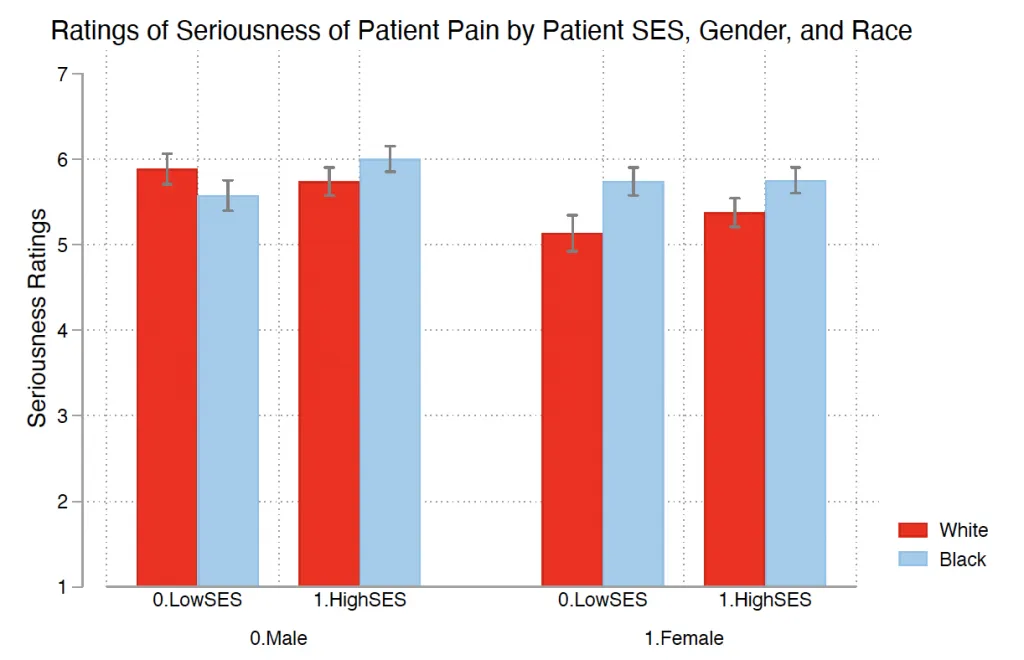
Implicit gender biases related to female pain certainly negatively shape the pelvic pain care experience, but such biases are only the tip of the iceberg when we are talking about the barriers patients face receiving care for pelvic pain. Experimental survey data also show patients from lower socioeconomic backgrounds have their pain rated as significantly less serious regardless of their gender. The same data also show patients with lower socioeconomic status (SES) have the credibility of their claims of pain questioned more intensely than higher SES patients.
Racial Biases
While patient race did not significantly impact evaluations of pain in my research, I did find that over half—51%—of survey respondents falsely believe Black people’s skin has more collagen and is therefore thicker than white people’s skin. Similarly, nearly half—49%—of respondents agreed with the false statement that Black people’s nerve endings are less sensitive than white people’s. While these endorsement of false beliefs of biological difference between Black and white people did not seem to impact evaluations of pain based on race according to my data, they remain an important piece of inquiry when it comes to racial biases and healthcare.
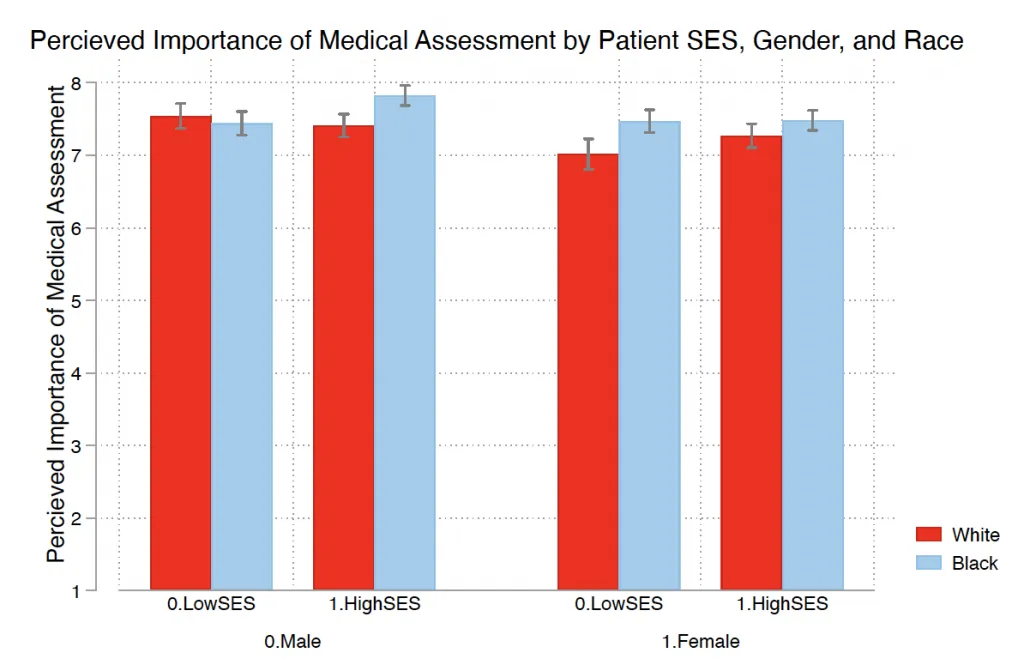
In the graphs below, you can see that when we look at how gender, race, and SES biases intersect, the issue becomes even more complex.
Decreasing Instances of Implicit Bias
Unfortunately, sociological knowledge tells us that fixing implicit biases will only fix one of many issues that, combined, create larger issues of health inequality in society. Even if we check our biases and no longer evaluate lower-SES patient pain as less serious than higher-SES patient pain, lower-SES patients will still face unique barriers to care.
For instance, the connection between employment and health insurance coverage will remain, leaving part-time workers without easy access to health insurance and therefore treatment. And even if we eradicated all racial bias in the world, the disproportionate placement of factories that emit harmful chemicals in Black neighborhoods would persist.
Final Thoughts on Implicit Bias in Pain Medicine
While checking our biases may not fix everything, it’s still necessary for treating each other with dignity and respect, whether we are treating patients or simply interacting with someone new for the first time on the street. Taking someone at their word when it comes to the pain they are experiencing, regardless of their gender, race, or SES, can do wonders for that patient’s experience. As a healthcare provider, giving patients that validation could make the difference between them continuing to seek care and giving up on finding relief.
So, next time you have a patient, friend, or acquaintance confide in you about their persistent pain, think about what biases you might be bringing to that interaction and the ways you can challenge them right then and there.